.
Whether you are personally struggling with an obsessive-compulsive condition or supporting someone who does, this pack has been designed to support you to navigate the NHS mental health system and understand what should be happening at each step. Accessing treatment can be a challenge, especially if the professionals you are speaking to don’t know what the best action to take is. Often, getting the right support can come down to knowing what someone is entitled to and how to ask for it.
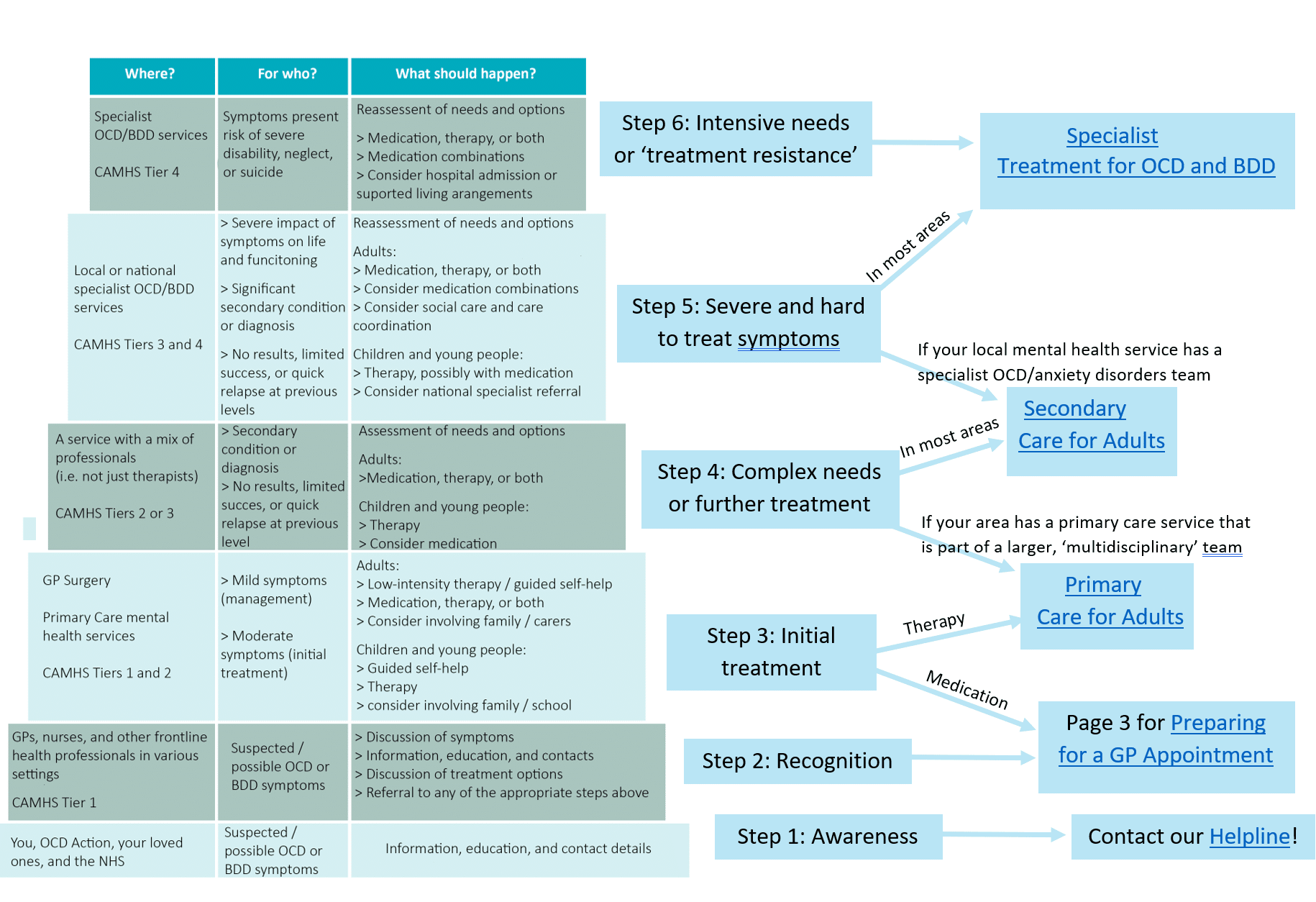
You can use the chart below to find where you or your loved one fit in the ‘stepped care’ system, and which of our factsheets might be most useful to read through. The table is a basic-language version of the one that can be found in the NICE ‘quick-reference’ version of the guidelines for OCD and BDD. The guidelines are clear that you do not have to start at the bottom and work your way up. Rather, you should be referred directly to the step that most fits your needs.
The links to the right can take you to our pages about the different steps. Primary and secondary care for children and adolescents are covered in our page about the Children and Adolescent Mental Health Services (CAMHS).
If the image is too small to read on your screen, you can right-click and select ‘Open image in new tab’ to see the full-size version.
The NICE guidelines for OCD and BDD
The National Institute for Health and Care Excellence (NICE) publishes guidelines for health and social care. Guidelines have been published for many conditions as well as particular practices, and they provide evidence-based recommendations and advice. These guidelines apply to England and Wales, but as Scotland and Northern Ireland don’t have their own OCD/BDD treatment guidelines, these are considered best practice and should still be followed.
Although the NICE guidelines are considered best practice, studies show that 25-30% of GPs don’t consider them particularly relevant and go against them on a regular basis. The guidelines are not legally binding, but through case law it can be considered medically negligent to ignore them. The decision to act against the guidelines must be supported by a reasonable body of experts. This can either be an already existing clinical practice that the doctor can refer to, or can come from a specialist assessment.
Put simply, this means that if the guidelines are clear and explicit about what you should be offered or how you should be treated, a doctor or service cannot take a different action simply because they disagree. They must be able to give a medical reason, and their individual opinion is not considered enough; it has to be backed up by something more official.
The guidelines for OCD and BDD are very in depth and clear, and we can help you to find yourself in them and put together information to show your doctor what should be happening. In most cases, this is all that is needed to move on to the appropriate next step in treatment.
If a doctor refuses to follow the guidelines, you can ask them to write that down in your medical record. You can specify that you want the note to reflect that you asked for the NICE-recommended treatment and were refused. You can also ask that your doctor provide you with a clear, written breakdown of their reasons for doing so.
If that still doesn’t work, you now have a list of reasons that you can appeal against. We can support you to put together your arguments and give you contact details for relevant people or organisations to contact about this in your area.