.
Secondary level healthcare is also sometimes referred to as ‘hospital and community care’. It involves more specialised services that offer emergency response and planned treatment for individuals with more severe or complex symptoms. You will need a referral from a primary care service (usually a GP) to access secondary care.
.
At this level
The secondary care mental health team is usually called the Community Mental Health Team (CMHT). This is a ‘multidisciplinary’ team, which simply means there are different types of professionals so that you can be offered the combination of services most appropriate for you.
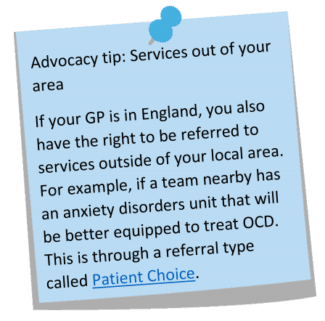 The team often have a base, like a clinic, that they work out of, but might also work in local hospitals, GP surgeries, or community centres. Most of the time a referral is made by the GP, but in some cases the primary care mental health team can also make the referral. At the very least, the primary care mental health team can recommend or request that your GP refer you on to secondary care.
The team often have a base, like a clinic, that they work out of, but might also work in local hospitals, GP surgeries, or community centres. Most of the time a referral is made by the GP, but in some cases the primary care mental health team can also make the referral. At the very least, the primary care mental health team can recommend or request that your GP refer you on to secondary care.
A CMHT might also include specialised teams within the larger service, which might be based in a separate building from the main team. These might cover specific conditions, like an eating disorder clinic, or specific groups of people, like those with learning disabilities. Some areas also have specific secondary care mental health services for young people ages 16-25.
.
Recommended by NICE
The NICE guidelines recommend secondary care treatment for any adult living with OCD who meets at least one of these three criteria:
- ‘Severe functioning impairment’, meaning the symptoms of OCD impact very strongly on your mental health, quality of life, and day to day activities like going to work and socialising.
- ‘Comorbidity’, meaning having more than one condition, which makes treating the OCD or engaging in the CBT more complex. If you don’t not have a second diagnosis you can request a mental health assessment, explaining why you believe you are struggling with more than one issue.
- ‘Poor or no response to initial treatment’, meaning you’ve tried high-intensity CBT with ERP from a primary care service but this wasn’t successful or enough.
The recommended treatment for OCD at this level of care is a combination of anti-obsessional medication and more intensive CBT with ERP. More intensive means more than 10 hours with a therapist/psychologist.
Remember that whether to try medication, therapy, or a combination of both is always an individual decision. You are entitled to choose to engage with just therapy or just medication if you prefer, regardless of what is offered or recommended.
Treatment at the Community Mental Health Team
 Assessment for treatment
Assessment for treatment
When you are referred for support or treatment through the CMHT, especially if referred for psychological treatment, you will be assessed by a mental health professional. The assessor will get a full picture of what you are experiencing and discuss treatment options. At this stage, if something different is offered, it can help to remember that CBT with ERP is the most effective treatment for OCD and what is recommended by the NICE guidelines.
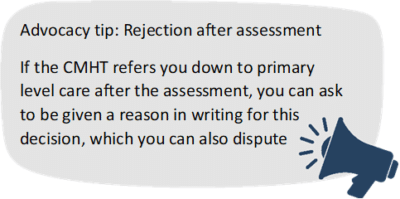
These types of assessment do not typically result in an official diagnosis, but the service can recognise OCD symptoms and acknowledge them in your records. After the assessment, you would either be placed on a waiting list or referred to a more appropriate service if the assessor does not believe the CMHT is the best option.- CBT with ERP with a Clinical psychologist
A clinical psychologist has years of training and experience working in the mental health system and offering psychological treatments to people with a range of needs. They will usually have a doctorate but are not medical doctors. They can offer more specialised CBT with ERP to you if you have severe symptoms or might be struggling with other problems that make the OCD harder to treat.
Often, clinical psychologists will have training in a number of psychological treatments. This usually includes CBT but that might not be the main therapy they are experienced in. What is important is that they have training in OCD and ERP, as outlined in the treatment guidelines. - Medication and Assessment for diagnosis with a Psychiatrist
A psychiatrist is a medical doctor who has specialised and trained in working with mental health conditions. The main services offered by psychiatry are assessment and medication. Your psychiatrist might also be the clinician overseeing your case, also known as your ‘consultant’.
If you haven’t responded to initial medication recommendations and are exploring more complex options like combinations, this will most likely be done with a psychiatrist. They might also be asked to consult on your medication as a one-off, while your GP remains in charge of prescribing and monitoring symptoms.
An assessment with a psychiatrist is a one-off appointment which would result in a report of your symptoms, a diagnosis, and recommendations for your treatment. These are quite rare and only needed if there is uncertainty about what you are struggling with.
- Mental health nursing and support
Community Psychiatric Nurses (CPN) and Mental Health Nurses (MHN) are trained in mental health and can offer you emotional and practical support, either at the CMHT or through home visits. Depending on their training and experience, this might include guiding you through CBT strategies or self-help resources for OCD. They can also give medication and monitor its effects. - Occupational Therapy
An Occupational Therapist (OT) provides assessments, information, and practical support around self-care, everyday tasks, work, and leisure to help an individual live independently. For example, if you are getting extra support at work because of your OCD, or have had to reduce your workload because of it, your employer might request an OT assessment. Their report would focus on the concrete and abstract obstacles brought on by your symptoms, as well as what adjustments would be appropriate. - Social services
Social workers bring a social perspective to the team’s working. They help people to talk through their problems, give them practical advice and emotional support, and can provide some psychological support such as CBT strategies. They are often able to give expert practical help with money, benefits, and housing issues.
Being under the care of a CMHT does not mean you will necessarily interact with a social worker. You should never be referred to social services only because of the themes of your intrusive thoughts, because these are not signs of risk. - Care coordination with any of the above
Also sometimes referred to as a key worker, a care coordinator is your main point of contact as a patient. They might speak to you regularly, monitor your mental health, offer information about the condition or services available, and, most importantly, coordinate your treatment plan and speak to professionals on your behalf. - Crisis support with the Crisis team
The crisis team offers short-term support aimed at preventing someone who is having a mental health crisis from needing hospitalisation. They can offer medication, home visits, and coping strategies, and should also support you to be in touch with other services for treatment and more long-term support. If you feel at risk of seriously hurting yourself you can get crisis support through your GP, calling 111, or calling your local urgent mental health helpline.
The NICE guidelines say that if you are ‘in remission’, which means your symptoms have improved and are not affecting your quality of life, you should be offered appointments over the next 12 months to monitor this. How often these will happen will depend on the individual case. If, after 12 months, you’ve kept up your recovery, you will be discharged back to your GP.
The NICE guidelines also offer specific steps as to what treatments and care should be offered at each stage, if the previous treatments didn’t work.
If the recommend treatment plan at this level (CBT with ERP combined with anti-obsessional medication) hasn’t brought on any or enough of a positive change in symptoms, then a multidisciplinary review is needed to discuss the next steps in your treatment, including the possibility of a referral to a specialist service.
If you have tried a combination of CBT with ERP and anti-obsessional medication, and within that have tried both an SSRI drug and Clomipramine, then the next step should be a referral to a multidisciplinary team with expertise in OCD or BDD.
This expert team should assess you and recommend a treatment plan. This might include more therapy, using medication combinations that are known to help boost the positive effects, or treatment through a specialist OCD/BDD treatment service.
