Note: This page has been made into new pages that are easier to follow along and have a little more information. If you would like to view those instead, you can find links on the left side of this page.
.
Specialist treatment services are available for individuals who have the most severe or complex symptoms of OCD and need to work with expert professionals or in intensive settings. They bring together professionals with experience in treating anxiety disorders, including OCD, and often in very severe forms.
While the treatment they offer doesn’t differ from other levels, these services specialise in working with people who have the most difficulty taking part in therapy. There are a number of national services for adults and children, and a few different options around how to get a referral and secure funding for the treatment.
Treatment options at this level
Depending on your needs, treatment history, and what treatment centre you are receiving care from, there are a few different treatment options at this level. The appendix below has more detailed information about each of the centres and what they offer.
This is usually done as a pre-curser to therapy, like with any other service. The assessor will get a full picture of what you are experiencing and discuss treatment options, then produce a report. The report will cover symptoms, diagnosis, and treatment recommendations. Sometimes, it can be easier for someone to get funding for just an assessment and use the report to get funding for the treatment.
Outpatient means that you are living at home throughout your treatment, and travel into the centre for therapy on a regular basis, generally once a week. If necessary, the services can also offer options if you can’t travel. They can work over video and sometimes offer home visits, until you are able to travel into the centre.
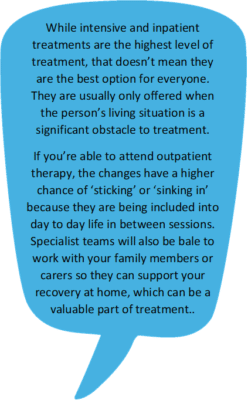 Inpatient means that you would be staying in the clinic for the duration of the treatment. Intensive means that you would be working with a professional multiple times a week, or even in a day.
Inpatient means that you would be staying in the clinic for the duration of the treatment. Intensive means that you would be working with a professional multiple times a week, or even in a day.
These are only offered in the most severe cases, for example when there is a high level of risk or self-neglect, or if your symptoms make it impossible for you to attend regular outpatient treatment.
Some of the services offer specialist medication advice for those who have struggled to find the right combination of medications so far. This is depending on the type of referral used.
Currently, neurosurgery is not recommended by NICE because of the limited improvement it has been found to bring. For a few very extreme cases, though, that small improvement can be what allows the recommended treatments to work. Very few people are offered neurosurgery per year.
The guidelines are currently under review and part of this will be considering new research on neurosurgery.
At the moment the only specialist centre that offers neurosurgery is the Advanced Interventions Service at Ninewells Hospital in Scotland. This is only available to people who have recently tried all of the recommended treatments at the highest level.
The NICE guidelines say that if you are ‘in remission’, which means your symptoms have improved and are not affecting your quality of life, you should be offered appointments over the next 12 months to monitor this. How often within these 12 months these will happen will depend on the individual case. If, after 12 months, you’ve has kept up your recovery, you will be discharged back to your GP.
Once the specialist treatment has been completed, you would usually be discharged back to your local services for monitoring of recovery. If you used Patient Choice to access the specialist treatment, your GP will need to refer you to the Community Mental Health Team (CMHT) for this. The specialist service should provide a plan or recommendations for your local team to follow.
The NICE guidelines also state that people who struggle with chronic or ‘treatment refractory’ OCD/BDD and haven’t improved through specialist treatment, “should have continuing access to specialist treatment services staffed by multidisciplinary teams of healthcare professionals with expertise in the management of the disorders”. This means that they should always be under the care of a secondary or higher level mental health team for ongoing support and treatment.
.
How to secure funding
Each local area has a designated Health Board that makes decisions about what services to fund. In England this is called the Clinical Commissioning Group (CCG). When someone needs an assessment or treatment from a service outside their local area, the Health Board must approve it first. The idea behind this is that your local area won’t pay extra for a service that isn’t needed, so you and your doctor need to show that it is. There are a few different pathways that can be used to secure funding for specialist treatment, depending on where you live and what service you need.
.
This is the ‘traditional’ referral pathway, usually led by your consultant at the Community Mental Health Team (CMHT).
If you are in Wales or Northern Ireland, this is the only pathway we are currently aware of.
If you are in England or Scotland, this is most appropriate if you need local mental health support while you wait for specialist treatment or alongside it. Examples of cases that require this are young people, individuals who are at significant risk of self-harm, or patients who have additional conditions that also require care.
The funding needs to be approved by the Local Health Board before you can go onto the waiting list with the specialist team. Your consultant will send a funding request for this. You can find information below on how to build a strong funding request with them.
NHS England and NHS Scotland have other funding pathways available for different situations, and which can be much easier to secure than with a traditional National Specialist funding request.
Currently the only service this can be used for is CADAT, at the Maudsley hospital in London. The Oxford Specialist centre is considering whether to accept this type of referral.
Patient Choice is a legal right under the NHS England constitution, which allows patients to choose where they want to receive treatment. This funding pathway can be used for any outpatient service that offers treatment for the condition you are struggling with, including some specialist ones.
This pathway is appropriate if you have severe symptoms but are not under the care of a local mental health team. If you are under the care of a mental health team, you would have to discharge yourself from it in order to use this option.
Through this pathway, a GP can refer you with a promise that your local area will fund the treatment if the services accepts you. This means that you can be put on a waiting list and seen for treatment straight away.
The National Services Division of NHS Scotland funds the specialist OCD service at the Ninewells hospital, in Dundee. This means that treatment at this service is already funded for Scottish residents. For more information on eligibility criteria for the Advanced Interventions Service, please see the appendix.
NHS England has a designated ‘pot of money’ that it can use to fund the treatment of the most serious and hard to treat cases. All the specialist services in the appendix are approved for HSS funding. NHS Scotland contributes to the pot, so Scottish residents are also eligible.
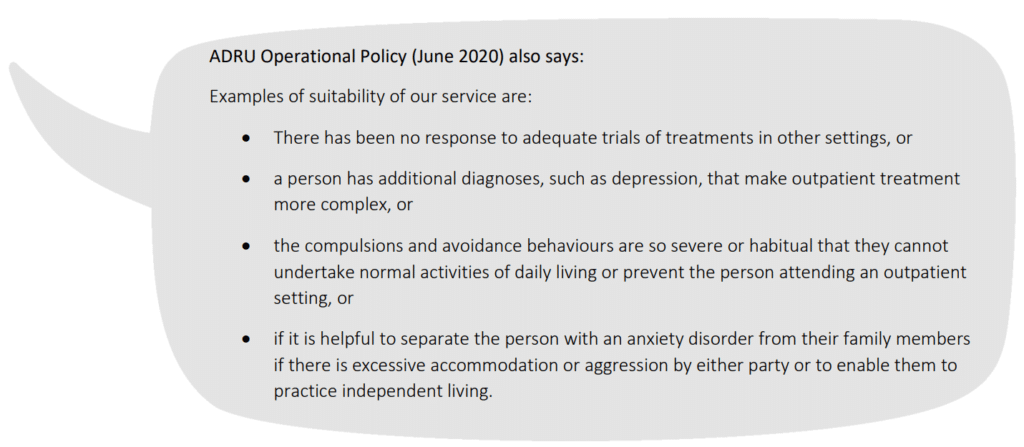
This pathway has much stricter requirements than others, but anyone who meets them will have the funding approved. To meet the criteria for this funding, you must meet all three of the following:
-
- A high score on an OCD or BDD scale
30 or above on Y-BOCS (for adults with OCD) and CY-BOCS (for children with OCD)
36 or above on the BDD-YBOCS (for people with BDD)
OR Your consultant can also provide a statement about how severe your symptoms are instead of a score - Unsuccessful treatment through therapy
2 rounds of ‘adequate’ CBT with EPR (for adults)
1 round of ‘adequate’ CBT with ERP (for children) - Unsuccessful treatment through medication
1 round of an SSRI (for children)
2 rounds of SSRIs, plus a round of augmentation, (for adults with OCD)
2 rounds of SSRIs (for adults with BDD)
OR if you are unable to take a full round of medication (3 months) because of your condition or because of the side effects you experience, the medication requirement can be dropped on a case by case basis
- A high score on an OCD or BDD scale
Putting together a strong funding request
No matter what pathway you chooses to use, a referral will be sent out to the service by a medical professional, outlining why they believe specialist treatment is necessary. If the specialist service agrees and the funding is in place, they will see you for an assessment, through which they’ll make their final decision.
If you are using the National Specialist or HSS funding options, your consultant must also put this argument forward to the funding board in order to secure funding. For HSS funding, the criteria above are quite specific, so the funding request just needs to clearly show that you meet those. Local Health Boards, on the other hand, will make the decision on a case by case basis. The most common reason given for refusing local funding is if you haven’t ‘exhausted local provision’. What this means is that, in most cases, you will have to have CBT through your local CMHT first, in order to show that more specialist CBT is necessary. It does not mean you have to try medication.
These types of requests are rare, so your consultant or GP might not know how to best put one together. You can see the referral and funding request before they are sent off, if you ask, so that anything that doesn’t best represent your situation can be changed.
Professionals might also be reluctant to make a referral because they worry it reflects badly on their team that they were not able to help. It can be helpful to bring along some information to back up why you think you need this referral:
- The NICE guidelines hold a lot of weight, because they are nationally recognised and professionals must be able to give a reason for going against them. The guidelines outline the stepped care model that specialist treatment is at the top of, so it can help to explain where on the steps you should be ‘slotted in’. If the clinician disagrees with where you believe you are on the scale, they have to be able to explain why in writing, if asked.
- Your full case history, including previous treatment, why previous treatment might have failed, and any documents that show your symptoms are entrenched or resistant to treatment so far (also called ‘treatment refractory’).
- A personal statement from you and/or your carer/s about how your symptoms impact your daily life (self care, activities, employment, education, relationships…) and mental health. OCD Action have a template letter than can be used for this and/or to request the referral.
- Information about the service you want a referral to and why this is different from local options. This can be their specialisation, which the NICE guidelines can provide some helpful quotes for, or data on how often the service is successful, which you can find on their website.
.
Trying again
Most people do have to push hard for this funding, so it’s to be expected to get some knock-back or to have to fight for it. It is important not to give up, and there are a number of things you can try if you haven’t been successful.
- It can be helpful to ask them to explain, in writing, their reasons for refusing. This gives you the chance to respond to their concerns or provide more information towards why it is necessary. It also means that they won’t be able to claim to have different reasons if challenged.
- Another option is to get assessed by an OCD/BDD specialist, and then use the assessment report to further back up the need for specialist treatment. This can be paid for privately, or you can ask to be referred for just the assessment as it will cost less – this is already included in the template letter linked above.
- A second opinion can also be requested, either from the specialist service (which funding would still need to be approved for) or from the local area. The Medical Director and Head of Psychology at the local Foundation Trust are two locally available roles that can provide a strong second opinion.
- If you are looking for a referral to the specialist services at the Maudsley hospital (CADAT or the Michael Rutter centre – see appendices), the clinic will generally make the funding referral for you. This means that all your consultant needs to do is fill out the referral form and send it off. Letting them know this, and that they won’t have to convince the Local health Board themselves, can be quite convincing.
Your Local Health Board should always give a written explanation for this, which can then be used to make any changes or additions to the request. The request can be sent through again as long as there has been a ‘material change in circumstances’, which includes adding more evidence and information to it.
There are also a number of people or organisations that can support you through this process or if you come across any obstacles that shouldn’t be there:
- If the Health Board’s decision or actions seem to be against their funding protocol or criteria, the rejection can be appealed to the Independent Funding Appeal Panel. Different local areas each have their own set of protocols, and you can ask to see the ones for yours.
- Although the reason for the decision should be sent through in writing, if you or your consultant have any other questions or want more detail, you can call or write to the decision makers directly to find out more about why.
- If the rejection seems to be because the information was not presented to the board well enough, a complaint can be made directly or through the Patient Advice and Liaison Service (PALS, might go by a different name in your area), which can offer mediation with the health professional.
- In some cases, when things just don’t seem to be moving along as they should, contacting the local Assembly Member or Member of Parliament can be helpful.
After specialist treatment
Once the specialist treatment has been completed, you would usually be discharged back to your local services for monitoring of recovery. If you used Patient Choice to access the specialist treatment, your GP will need to refer you to the Community Mental Health Team (CMHT) for this. The specialist service should provide a plan or recommendations for your local team to follow.
The NICE guidelines say that if you are ‘in remission’, which means your symptoms have improved and are not affecting your quality of life, you should be offered appointments over the next 12 months to monitor this. How often these will happen will depend on the individual case. If, after 12 months, you’ve kept up your recovery, you will be discharged back to your GP.
The NICE guidelines also state that people who struggle with chronic or ‘treatment refractory’ OCD/BDD and haven’t improved through specialist treatment “should have continuing access to specialist treatment services staffed by multidisciplinary teams of healthcare professionals with expertise in the management of the disorders”. This means that they should always be under the care of a secondary or higher-level mental health team for ongoing support and treatment.
.
Appendix: Specialist centres in the UK
Including ‘CADAT-PAX’ (Parents with AnXiety) unit
Postal address:
Centre for Anxiety Disorders and Trauma,
The Maudsley Hospital,
South London & Maudsley Trust,
99 Denmark Hill,
London,
SE5 8AZ
Telephone: 020 3228 2101
Email addresses:
CADAT@slam.nhs.uk (general queries)
cadatreferrals@slam.nhs.uk (for referrals)
More details about the information below:
https://www.slam.nhs.uk/national-services/adult-services/centre-for-anxiety-disorders-and-trauma/
Care options–
(Based on treatment needs, referral type, and location)
- Outpatient CBT for OCD, BDD, and Hoarding Disorder (12-20 sessions)
- Home-based CBT for OCD and BDD (12-20 sessions)
- For Hoarding Disorder specifically in Lambeth, Southwark, and Lewisham
- Intensive CBT for OCD, BDD, and Hoarding Disorder (1 week of treatment)
- Medication advice for individuals funded by HSS
- ‘Team assessment’ – Treatment recommendations to your local mental health team
Who the service is for–
- Adults whose main psychological concern is an anxiety or trauma condition (or both)
- OCD, BDD, HD, PTSD, Depersonalisation, Mysophonia, other panic/anxiety/phobic conditions
- If taking medication, must be a ‘stable dose’ – meaning you aren’t currently testing out different tablets and dosages
- If you are pregnant or a parent of a child under 4yo you will be seen through CADAT-PAX, which has a shorter waiting list and specialises in this period of life
How to get a referral–
You can download the referral form by clicking here
GP in Lambeth, Southwark, and Lewisham:
Do not use the form unless you are applying through HSS (see below)
- CADAT is included within your local services so is already funded for suitable referrals. You can self-refer directly to your local IAPT, because the centre offers treatment at all levels. IAPT will triage you so make sure to make it clear that you are struggling with and obsessive-compulsive condition at the screening and assessment, and you can ask about a referral to CADAT if you want to.
Lambeth 0203 228 6747
Lewisham 0203 049 2000
Southwark 0203 228 2194
Bexley, Bromley, and Greenwich residents:
- Funding only available through your local CCG. See ‘National Specialist’ option below
Other England residents:
- Patient Choice (if you are not under the care of a mental health team)
GP fills out the form, including ‘Patient Choice only’ section at the top of page 3, confirming you meet the criteria listed in that section.
CADAT receives the referral form, and can immediately add you to their waiting list. - Highly Specialised Service (HSS, if you have had lots of unsuccessful recommended treatment)
Consultant (usually psychologist/psychiatrist) fills out the form, including ‘Treatment Resistant Obsessive Compulsive Disorder / Body Dysmorphic Disorder Service’ Section on pages 3 and 4, confirming you meet the criteria for that section.
CADAT receives the referral form, and may assess you. If they agree that you meet the criteria for HSS (national funding from NHS England) they will apply to the funding for you. - National Specialist (if you cannot use the other options)
Consultant (usually psychologist/psychiatrist) fills out the form, including ‘National Specialist’ section on page 3, confirming you meet the criteria listed in that section.
CADAT receives the referral form, and will do the funding request for you.
*In some areas* the CCG will require that your consultant does the funding request instead. If this is the case, CADAT will let them know.
Wales and Northern Ireland residents:
- Funding only available through your Local Health Board
Consultant (usually psychologist/psychiatrist) fills out the form, including ‘National Specialist’ section on page 3, confirming you meet the criteria listed in that section.
If you aren’t under a Community Mental health Team, your GP can do the referral but must confirm that you don’t need local support for complex needs.
CADAT receives the referral form, and will do the funding request for you.
*In some areas* the health funding board will require that your doctor does the funding request instead. If this is the case, CADAT will let them know.
Scotland residents:
- National Specialist (if you don’t meet the HSS criteria)
Your consultant (usually psychologist/psychiatrist) fills out the form, including ‘National Specialist’ section on page 3, confirming you meet the criteria listed in that section.
If you aren’t under a Community Mental health Team, your GP can do the referral but must confirm that you don’t need local support for complex needs.
CADAT receives the referral form, and will contact your local health board to request the funding.
*In some areas* the health board will require that your doctor does the funding request instead. If this is the case, CADAT will let them know. - Highly Specialised Service (HSS, if you have had lots of unsuccessful treatment)
Your consultant (usually psychologist/psychiatrist) fills out the form, including ‘Treatment Resistant Obsessive Compulsive Disorder / Body Dysmorphic Disorder Service’ Section on pages 3 and 4, confirming you meet the criteria for that section.
CADAT receives the referral form, and may assess you. If they agree that you meet the criteria for HSS (national funding from NHS England, which Scotland contributes to) they will apply to the funding for you.
Postal address:
Oxford Health Specialist Psychological Intervention Centre
Warneford Hospital
Headington
Oxford
OX3 7JX
Telephone: 01865 226361
Email address:
ohspic@oxfordhealth.nhs.uk
More details about the information below:
https://ohspic.web.ox.ac.uk/
Care options–
(Based on treatment needs, referral type, and location)
- Outpatient CBT for OCD and Hoarding Disorder
- Home-based or ‘outreach’ CBT for OCD and Hoarding Disorder
- Intensive CBT for OCD and Hoarding Disorder
- Medication advice
- ‘Team assessment’ – Treatment recommendations to your local mental health team
Who the service is for–
Adults and children whose main psychological concern is an anxiety or trauma condition (or both)
- OCD, Hoarding Disorder, PTSD, other panic/anxiety/phobic conditions
- If there is also a secondary condition outside of these (like BDD or ASD), care for this will be considered as well
How to get a referral–
Whole of UK. You can read about this in more detail here
- An NHS healthcare professional who knows your case well fills out the referral form and adds a referral letter outlining any further information and treatment documentation
- The clinic lets the referrer know whether the referral is appropriate and how much an assessment will cost. They will provide a ‘Funding Approval Form’ (FAF)
- Your referrer makes a request for funding from your Local Health Board. If approved, the health board will confirm this by filling out the FAF
- You will be assessed through a single, 2-3 hour appointment. Within 3 weeks, the clinic will send a report to your referrer, outlining their treatment recommendations and the cost of this. They will again provide a FAF for this
- Your referrer makes a second request to the Health Board, this time for the treatment funding. Again, your Local Health Board will fill out the FAF if they approve it
- You will be put on a waiting list for treatment, which will start within 18 weeks
The centre is currently considering whether to accept Patient Choice referrals.
Postal address:
Dower House
Bethlem Royal Hospital
Monks Orchard Road
Beckenham
Kent
BR3 3BX
Telephone: 01865 226361
Email address:
Anxiety.DisordersResidentialUnit@slam.nhs.uk
More details about the information below:
https://www.slam.nhs.uk/national-services/adult-services/anxiety-disorders-residential-unit/
Care options–
(Based on treatment needs, referral type, and location)
- Residential treatment for OCD and BDD (average 12-16 weeks)
- Different from inpatient because unstaffed evenings and nights
- CBT, occupational therapy, regular reviews, group work
- Relapse prevention plan as part of discharge
- Second opinion assessment for complex cases
Who the service is for–
- Adults whose main psychological concern is an anxiety or trauma condition (or both)
- OCD, BDD, PTSD, other panic/anxiety/phobic conditions
- You must be able to travel home on weekends – meaning having a place you can stay and an ability to travel (independently or with your own support)
- You must be able to perform basic self-care and self-medicate
- Cannot be struggling with current issues of psychosis, addiction, or high risk behaviour that need your own care or treatment
How to get a referral–
You can download the referral form by clicking here
Whole of UK
- National Specialist (if you don’t meet the HSS criteria)
Your consultant (usually psychologist/psychiatrist) would send a completed referral form for assessment and/or treatment to the unit, outlining your symptoms and treatment history.
Your consultant also needs make a funding request to your Local Health Board. This can be done beforehand or alongside, but you cannot be placed on a waiting list until the funding is approved. - Highly Specialised Service (HSS, if you live in England or Scotland and have had lots of good quality but unsuccessful treatment)
Your consultant (usually psychologist/psychiatrist) would send a completed referral form for assessment and/or treatment to the unit, outlining your symptoms and treatment history.
They would also make a funding request to NHS England, outlining how you meet the HSS criteria. This can be done beforehand or alongside, but you cannot be placed on a waiting list until the funding is approved.
Postal address:
National OCD/BDD Service
Springfield University Hospital
61 Glenburnie Road
Tooting
London
SW17 7DJ
Telephone: 020 3513 6961
Email address:
ocdbdd@swlstg.nhs.uk
More details about the information below:
https://www.swlstg.nhs.uk/our-services/specialist-services/ocd-bdd-service
Who the service is for–
Adults whose main psychological concern is OCD, BDD, or Hoarding Disorder.
Care options–
Read more on all of these here
Trustwide Service (OCD/BDD)
Read more here
Your GP or consultant (psychiatrist/psychologist) can ask for support from one of the therapists in the service. This can be:
- Support and guidance for the mental health professionals who work with you
- Joint working with your team and delivering therapy as part of your care plan
- Treatment for you directly from the service in your home or as an outpatient
The usual criteria for this service is to have tried 1 round of CBT and 2 rounds of medication unsuccessfully, but if your case is clearly quite severe or complex, they might consider you without these having been met.
National Services (OCD/BDD/HD)
(Based on treatment needs, referral type, and location)
- Outpatient/community CBT
- Home-based CBT
- Inpatient treatment
- Appropriate for people who are not able to self-care independently
How to get a referral–
You can find the referral forms for the different services here
Whole of UK
- National Specialist (if you don’t meet the HSS criteria)
Your consultant (usually psychologist/psychiatrist) would send a completed referral form for assessment and/or treatment to the unit, outlining your symptoms and treatment history.
Your consultant also needs make a funding request to your Local Health Board. This can be done beforehand or alongside, but you cannot be placed on a waiting list until the funding is approved. - Highly Specialised Service (HSS, if you live in England or Scotland and have had lots of good quality but unsuccessful treatment)
Your consultant (usually psychologist/psychiatrist) would send a completed referral form for assessment and/or treatment to the unit, outlining your symptoms and treatment history.
They would also make a funding request to NHS England, outlining how you meet the HSS criteria. This can be done beforehand or alongside, but you cannot be placed on a waiting list until the funding is approved.
through the Hertfordshire Partnership University NHS Foundation Trust
Postal address:
Prof NA Fineberg
Consultant Psychiatrist
Rosanne House
Parkway
Welwyn Garden City
AL8 6HG
More details about the information below:
https://www.hpft.nhs.uk/services/community-services/highly-specialised-services-for-obsessive-compulsive-disorders-ocds-and-applied-neuroscience/
Care options–
- Outpatient CBT for OCD, BDD, Hoarding Disorder, and BFRB
- Inpatient CBT for OCD, BDD, Hoarding Disorder, and BFRB
- Medication treatment for OCD, BDD, Hoarding, and BFRB
- Outreach for people admitted onto psychiatric wards at Hertfordshire Partnership University NHS Foundation Trust and inpatient units elsewhere in England, including for people receiving treatment under the mental health act
- Assessment for neurosurgery
Who the service is for–
- Adults whose main psychological concern is OCD or a related condition (including Hoarding Disorder and BFRB) at levels 4-6 on the stepped care chart
- Needs, criteria, and cost of treatment will be discussed individually
How to get a referral–
Whole of UK
- National Specialist (if you don’t meet the HSS criteria)
Your consultant (usually psychologist/psychiatrist) would send a completed referral form for assessment and/or treatment to the unit, outlining your symptoms and treatment history.
Your consultant also needs make a funding request to your Local Health Board. This can be done beforehand or alongside, but you cannot be placed on a waiting list until the funding is approved. - Highly Specialised Service (HSS, if you live in England or Scotland and have had lots of good quality but unsuccessful treatment)
Your consultant (usually psychologist/psychiatrist) would send a completed referral form for assessment and/or treatment to the unit, outlining your symptoms and treatment history.
They would also make a funding request to NHS England, outlining how you meet the HSS criteria. This can be done beforehand or alongside, but you cannot be placed on a waiting list until the funding is approved.
Postal address:
National OCD/BDD Service
Springfield University Hospital
61 Glenburnie Road
Tooting
London
SW17 7DJ
Telephone:
0808 159 8296
020 8023 6799
Email address:
Priory.Referral@nhs.net
More details about the information below:
https://www.priorygroup.com/nhs/locations/priory-hospital-north-london-nhs-services
 Care options–
Care options–
- Inpatient treatment for OCD and BDD
-
- One to one and group
- General psychology groups also available during stay
-
Who the service is for–
- Adults and adolescents (12+) whose main psychological concern is OCD or BDD
How to get a referral–
Whole of UK
- National Specialist (if you don’t meet the HSS criteria)
Your consultant (usually psychologist/psychiatrist) would send a completed referral form for assessment and/or treatment to the unit, outlining your symptoms and treatment history.
Your consultant also needs make a funding request to your Local Health Board. This can be done beforehand or alongside, but you cannot be placed on a waiting list until the funding is approved. - Highly Specialised Service (HSS, if you live in England or Scotland and have had lots of good quality but unsuccessful treatment)
Your consultant (usually psychologist/psychiatrist) would send a completed referral form for assessment and/or treatment to the unit, outlining your symptoms and treatment history.
They would also make a funding request to NHS England, outlining how you meet the HSS criteria. This can be done beforehand or alongside, but you cannot be placed on a waiting list until the funding is approved.
Private inpatient treatment is also available
Advanced Interventions Service
Area 7, Level 6
South Block
Ninewells Hospital and Medical School
Dundee
DD1 9SY
Telephone: 01382 496233
Email address:
enquiries@advancedinterventions.org.uk
More details about the information below:
https://www.advancedinterventions.org.uk/
Care options–
- Assessment with treatment advice for your local team
- Intensive inpatient or home-based CBT with ERP for OCD
- Neurosurgery (Anterior Cingulotomy)
- Inference-Based Therapy (OCD Action does not have any further information on this treatment)
Who the service is for–
- Adults whose main psychological concern is OCD at levels 5 or 6 on the stepped care chart
Usually expected to have tried multiple rounds of CBT and medication
How to get a referral–
Read more about the referral process, guidelines, and criteria here
For Scottish residents, the consultant (usually psychologist/psychiatrist) just needs to write to the service with information about your condition and treatment history. The funding for this service is provided by the National Services Division.
Rest of UK
- National Specialist (if you don’t meet the HSS criteria)
Your consultant (usually psychologist/psychiatrist) would send a completed referral form for assessment and/or treatment to the unit, outlining your symptoms and treatment history.
Your consultant also needs make a funding request to your Local Health Board. This can be done beforehand or alongside, but you cannot be placed on a waiting list until the funding is approved. - Highly Specialised Service (HSS, if you live in England and have had lots of good quality but unsuccessful treatment)
Your consultant (usually psychologist/psychiatrist) would send a completed referral form for assessment and/or treatment to the unit, outlining your symptoms and treatment history.
They would also make a funding request to NHS England, outlining how you meet the HSS criteria. This can be done beforehand or alongside, but you cannot be placed on a waiting list until the funding is approved.
Postal address:
Michael Rutter Centre
De Crespigny Park
London
SE5 8AZ
Telephone: 020 3228 5222
Email address:
ocdbdd.camhs@slam.nhs.uk
“Families, GPs, and referrers are welcome to contact us for information.”
More details about the information below:
OCD Service
BDD Service
Care options–
- Outpatient CBT for OCD (14-20 sessions avg.), BFRB, and BDD (20 sessions avg.). Also ASD, tic conditions, and other anxiety disorders
- Where appropriate, will include and work with parents/carers
- Remote options like telephone and video available
- Some inpatient and outreach treatment
- Medication treatment
- ‘Team assessment’ – Treatment recommendations to your local mental health team
- Follow-up appointments for a year after treatment
Who the service is for–
- Young people (up to 18) with a suspected diagnosis of OCD, BFRB, BDD
- Must be under the care of a local mental health team
 How to get a referral–
How to get a referral–
Read more about what goes into a referral here
Whole of UK
- National Specialist
Your consultant (usually psychologist/psychiatrist**) would send a completed referral form for assessment and/or treatment to the service, outlining your symptoms and treatment history.
When the service receives the referral form, they will contact your Local Health Board to apply to the funding for you.
In some areas the health board will require that your doctor does the funding request instead. If this is the case, the service will let them know.
**If your GP knows your case best or is more helpful, they can make the referral. CAMHS must be involved and has to support the referral, but this might be easier to convince them to do. - Highly Specialised Service (HSS, for people in England or Scotland who have had lots of good quality but unsuccessful treatment)
Your consultant (usually psychologist/psychiatrist**) would send a completed referral form for assessment and/or treatment to the service, outlining your symptoms and treatment history.
When the service receives the referral form, they may assess you. If they agree that you meet the criteria for HSS they will apply to the funding for you.
**If your GP knows your case best or is more helpful, they can make the referral. CAMHS must be involved and has to support the referral, but this might be easier to convince them to do.