Laura Johnson: scientist, mum of two, and the doodler behind OCD Doodles tells us all about her experience of seeking treatment for OCD, from an unlicensed coach to a national specialist centre for OCD.

I was on holiday with my family, celebrating my daughter’s first birthday when I felt I couldn’t cope with my maternal OCD anymore.
The harm thoughts were relentless and whilst staying with my parents and in-laws, I could no longer hide my compulsions or hurt. I was unable to control anything the way that my OCD demanded. Family members were handing my daughter things that I perceived to be contaminated, she was being kissed and breathing in air that my OCD deemed ‘disgusting’. My OCD was screaming at me and I was trying to stay silent. Silently neutralising the thoughts, ruminating and wishing the holiday to be over. What was supposed to be a break, felt like anything but.
It was at that point that I broke down. Shaking, I turned to my family and shouted, “Nobody can look after her like I can, nobody understands!”. I felt terrible, what had I done? The last thing I wanted to do was to insult or hurt the people that I loved, but the critical, dominating voice that told me that I must protect my daughter at all costs had become too loud to keep inside. I couldn’t accept help from family, from formula milk, medication, not from anyone or anything. I doubted everyone, my own intentions and senses. It was all on me and I was exhausted. In that moment, I cried, I kicked, and I screamed. And then I showered to try to wash away the guilt, shame, and mental contamination that I felt so viscerally. My mum wanted to take me to the hospital then and there but once the wave of anxiety had passed, I promised that I would seek specialist help.
“I told several GPs, therapists, and university counsellors but nobody picked up on my OCD symptoms.”
I had first opened up about my mental health a decade earlier. I told several GPs, therapists, and university counsellors but nobody picked up on my OCD symptoms. Furthermore, I was under the impression that I knew what OCD was and I didn’t fit the stereotype. It wasn’t until I was 3 months pregnant with my daughter, at the age of 29, that an IAPT therapist told me that OCD was responsible for the symptoms I’d experienced since childhood. Whilst I was incredibly grateful to finally put a name to my intrusive thoughts and compulsive behaviours, I received little in the way of exposure work during the following twenty therapy sessions. I think my depression benefitted from talking to somebody, but I didn’t make much progress with the OCD and my symptoms continued to get worse during my daughter’s first year. Although I had promised to seek specialist help, I was scared that treating the OCD would make me a riskier person and I thought that I had exhausted all options for treatment with the NHS.
“I was vulnerable and desperate, so the promise of a 100% recovery was music to my ears. I thought I’d found the key.”
Eventually, six months later, when I realised the disorder really wasn’t going to go away by itself, I turned to Instagram to see if there were other people experiencing similar symptoms. I needed hope and to know that I wasn’t alone. It was at this point that I was approached by an ‘OCD coach’ who claimed to be an ‘expert by experience’. The coach’s social media posts really spoke to me. I could tell that this person really understood how it felt to suffer with OCD. They claimed to be fully recovered and used the inadequate care that I had received previously to convince me that nobody else really understood. I was vulnerable and desperate, so the promise of a 100% recovery was music to my ears. I thought I’d found the key.
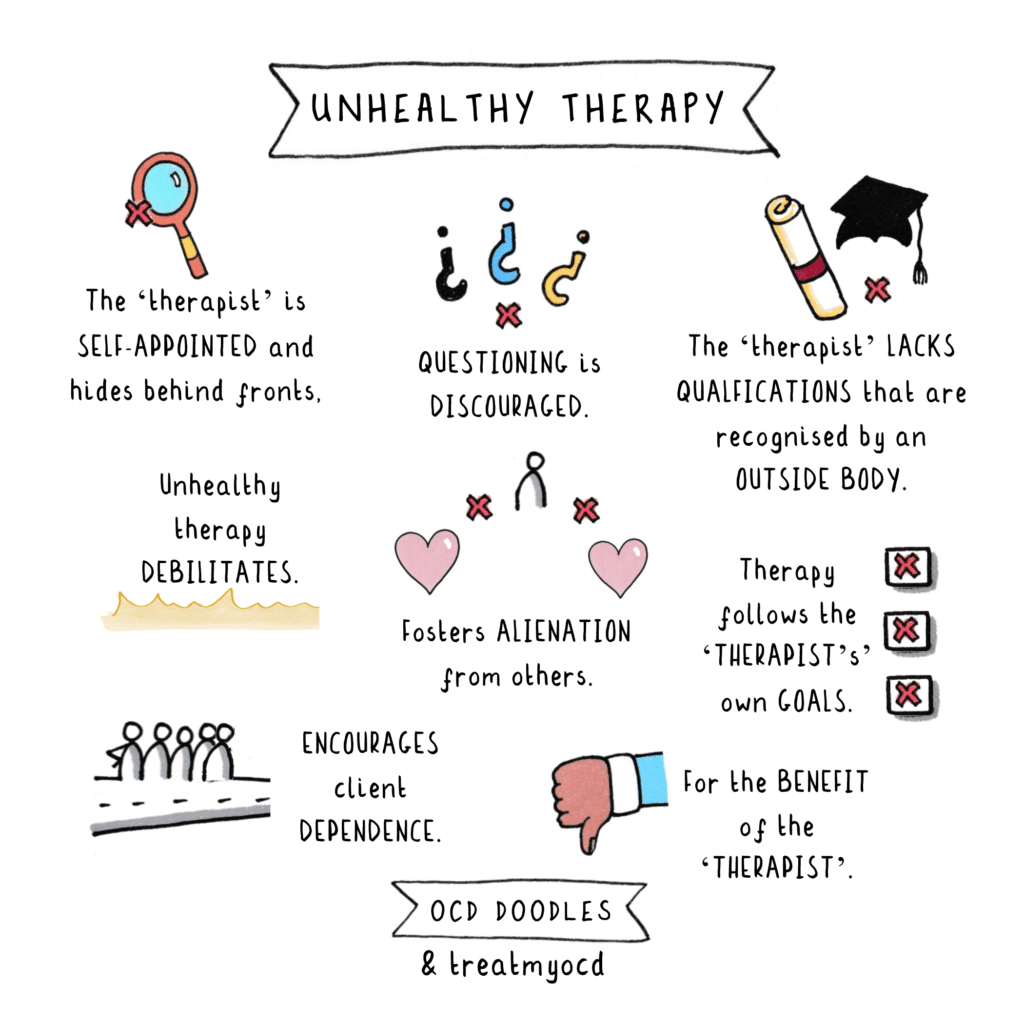
I spent 9 months in ‘treatment’ with this person, learning the basics of Albert Ellis’ ABC model and unknowingly trying to compulsively rationalise my way out of my obsessions. I was told to do extreme exposures and shame attacks, with very little knowledge of response prevention. I found these experiences so stressful that they’d often induce a migraine and leave me unfit to drive home. A plethora of ethical issues were plain to see from the outside, but I was ignorant to them, I was scared to give up what I had been told was my only chance of recovery.
By this point I had lost all hope. The unqualified coach had tried to turn me against qualified therapists, psychiatrists, the online OCD community, and charities. But one day, I saw a post by an American therapist detailing why ‘experts by experience’ are not qualified to treat OCD. I somehow summoned the courage to leave the support groups and block the coach.
When I became pregnant with my second child, I decided I would take all the professional help that I could get. I was referred to IAPT and the perinatal mental health team. I had another twenty sessions of CBT through IAPT, but these focused mainly on my past and what the root cause of my thoughts might be. Unfortunately, again, I did very little exposure work. I saw another psychotherapist, a psychiatrist, psychologist, a CPN and specialist midwife during my second pregnancy and the postpartum period. I felt very supported, and I was grateful to have people to talk to, but they were concerned that exposure work might be harmful whilst I was pregnant and when my son was 6 months old, Coronavirus affected their services.
“The day I picked up the phone was the day that everything changed, and I started on the path to specialist OCD treatment. How I wish I’d called sooner!”
I found myself turning more and more to books by OCD specialists, the OCD Stories podcast, and articles written by OCD charities. I had thought about calling OCD Action several times but always ended up doubting my diagnosis and feeling like I didn’t know what to say, but the day I picked up the phone was the day that everything changed, and I started on the path to specialist OCD treatment. How I wish I’d called sooner!
I joined OCD Action’s Next Steps program and when the perinatal mental health therapy finished, an OCD Action volunteer gave me the information that I needed to access a national OCD service through a type of referral called Patient Choice.
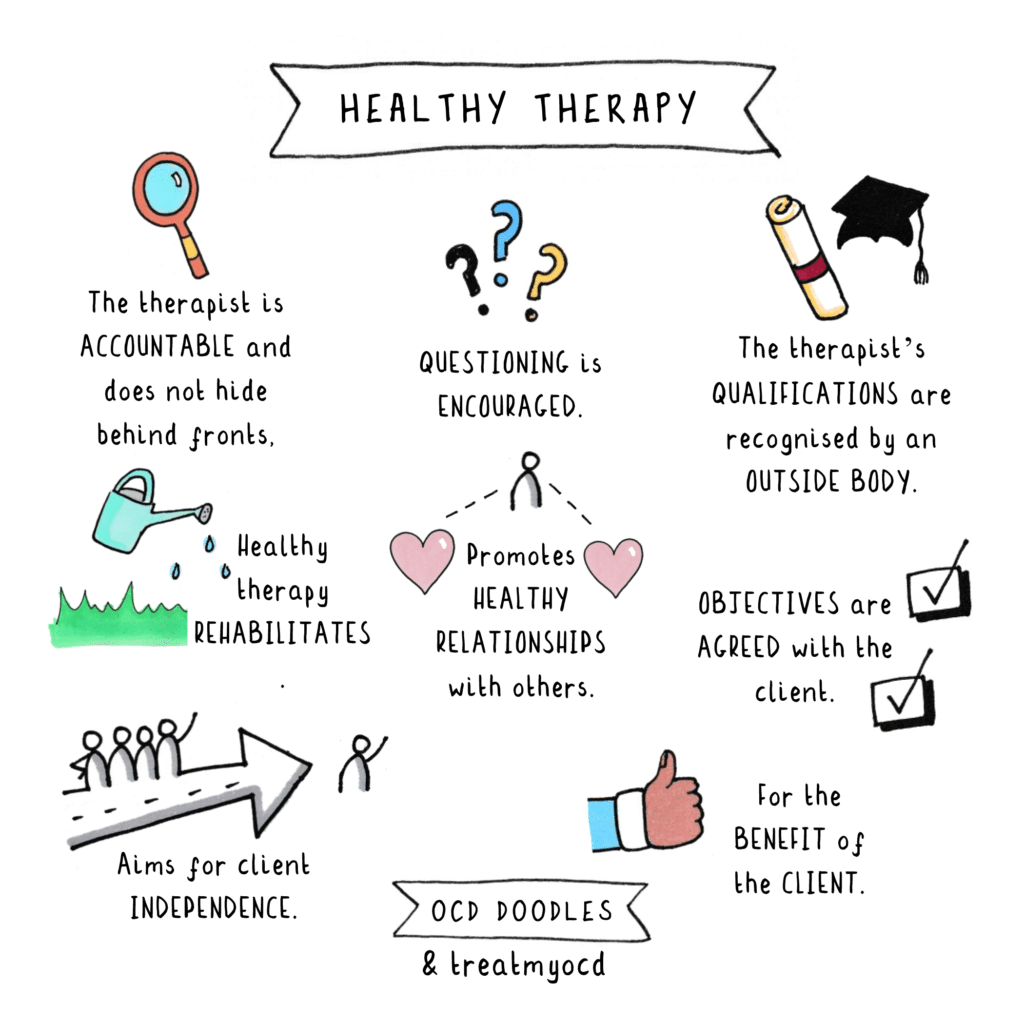
I was referred for teletherapy with the CADAT-PAX service at the Maudsley. I received a thorough mental health assessment and structured course of Exposure and Response Prevention (ERP) therapy which gave me the tools I needed to face my fears and resist my compulsions in a healthy and productive way.
I am so grateful to the OCD Action volunteer who spent hours on the phone to me, listening, without judgment, gently guiding me toward the information that got me to the care I needed. If I’d called OCD Action sooner, I don’t think it would have taken me a further 5 years, post-diagnosis, to receive a course of ERP. For the first time in many years, I feel confident in my relapse prevention plan and hopeful for the future.
CBT with ERP vs. Coaching
In my experience, the difference between therapy led by an OCD specialist versus therapy led by an unqualified coach was vast. During treatment with the unqualified coach there was a clear lack of ethics, boundaries, compassion, and trust. I was asked to produce videos performing distressing exposures which were later shared on social media, I was offered free sessions in return for glowing testimonials, and I was paraded as a success story to ‘give others hope’ when I was still suffering. Furthermore, the sessions cost a lot of money. I was one of the first to be treated by this person when sessions were £80 per 50-minute session. They are now in excess of £300. I had over 20 sessions and paid more than £2,000. I know people that have paid over £9,000 for the same sessions, which often lasted between 5 and 15 minutes.
I don’t think I can overstate how important it is to have a therapist that is trustworthy, ethical, professional, qualified, sets boundaries, and crucially, understands OCD. The coach that I worked with claimed to have ‘the best recovery rates’. They said they were one of only a handful of people who truly understood OCD. When asked to provide evidence of his claims, clients were manipulated and told that he was their ‘only chance of recovery’. As a scientist who is educated about ethics and values qualifications, I still struggle to believe that I got caught up in such terrible treatment. However, as a person that was suffering and feeling desperate for a solution, I know I was willing to try anything to stop what I was experiencing. Even when family members voiced their concerns about the treatment, I was very much distracted by the promise of a full recovery.
For information on good quality CBT with ERP and what to look for in a therapist, head to the resources section on OCD Action’s website.